HPV infections drop due to widespread vaccination
Human papillomavirus (HPV) is the most common sexually transmitted infection in the US. Although most genital HPV infections are harmless, at least a dozen types can lead to cancer. Strains 16 and 18 cause an estimated 70% of cervical cancers and represent two of nine strains covered by the HPV vaccine.
In an analysis published in the Centres for Disease Control and Prevention (CDC) Morbidity and Mortality Weekly Report in late March, Rosenblum and colleagues found that the US’s HPV vaccination programme has led to declines in infections among both vaccinated and unvaccinated women and girls.
GlobalData epidemiologists expect these declines in infection will translate to decreases in associated cancers, including cervical cancer, in the US.
Rosenblum and colleagues used data from the National Health and Nutrition Examination Survey (NHANES), an ongoing CDC national survey, through 2018 to examine HPV prevalence among vaccinated and unvaccinated women.
They found that the prevalence of the strains targeted by the vaccine was 88% lower among females aged 14-19 years from 2015 to 2018 compared with the pre-vaccine era (2003 to 2006), and 81% lower among females aged 20-24 years.
Prevalence was also lower among unvaccinated females, suggesting a strong herd immunity effect. These findings accounted for race, ethnicity and potential changes in sexual behaviour over the study period.
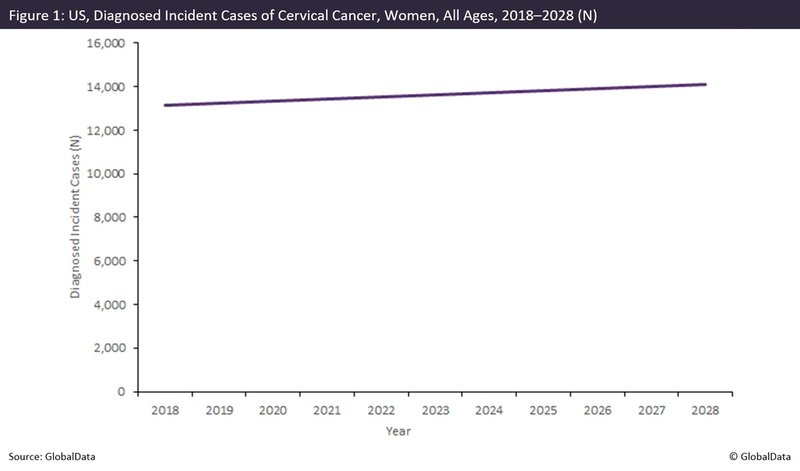
GlobalData epidemiologists forecast that the diagnosed incident cases of cervical cancer will increase in the US, exceeding 14,000 cases in 2028 (as shown by the graph below).
But as HPV infection prevalence will continue to decrease due to the vaccination efforts, a corresponding decline in new cases of cervical cancer will probably follow.
The number of incident cases may, therefore, be lower than expected for the latter part of the forecast, although it may take some time to see the impact of HPV vaccination on cervical cancer rates because of the 15-20 year latency between infection and cancer development.
In the US, HPV vaccination is recommended for children aged 11-12 years. For adults who were not previously vaccinated, catch-up vaccination is recommended up to age 26 years.
While GlobalData epidemiologists recommend continued monitoring of trends in the prevalence of HPV and associated cancers, the evidence currently available suggests that the vaccine is an effective tool for the primary prevention of cancer.
For pharmaceutical industry data, comment and analysis, visit GlobalData's Pharmaceuticals Intelligence Centre.
Market Insight from