The mumps virus is highly contagious, spreading rapidly, and can lead to complications including meningitis, pancreatitis, and inflammation of the heart and ovarian/testicular swelling, to name just a few.
Once caught, the only option is treatment of the symptoms, and with sterility, deafness, and even risk of death from kidney and pancreatic complications listed as rare but potential outcomes, the preferable option is to prevent the disease in the first place. So with vaccine immunity waning, are the drugs we use today still good enough? We track the history of drug development for mumps.
5th century BC
First written description of mumps
The first written description of mumps as a disease can be found as far back as the 5th century BC. The father of medicine Hippocrates described an outbreak of mumps on the Greek island of Thasos in approximately 410BC, which modern physicians today still refer back to as a masterful documentation of the disease.
“Swellings appeared about the ears, in many on either side, and in the greatest number on both sides,” the passage reads. “They were of a lax, large, diffused character, without inflammation or pain, and they went away without any critical sign.”
The full description, contained within the Corpus Hippocraticum in the first book of the ‘Epidemics’, is often cited as an example of the value of observation in the process of disease treatment.
1934
Aetiology of mumps discovered
While various studies into the disease had been carried out across the 19th and 20th centuries, the viral aetiology of mumps was finally discovered and documented by Claud D. Johnson and Ernest W. Goodpasture in 1934.
Johnson and Goodpasture found that rhesus monkeys infected with a virus found in specimens of saliva taken from patients suffering from the early stages of the mumps went on to develop the disease themselves. They therefore judged that this virus was the cause of mumps, enabling new avenues of research to be opened up into the development of a vaccine to stop further spread of the disease.
1945
Isolating the mumps virus
In 1945 the mumps virus was first isolated, and by 1948 an inactivated vaccine had been developed. This version of the mumps vaccine only had short-term effectiveness however, with subsequent preparations utilising a live virus that has been weakened, rather than an inactivated variety.
This version of the vaccine was relatively short-lived, and was discontinued in the mid-1970s as more effective options were developed.
1967
Mumpsvax: the Jeryl Lynn vaccine
On 30 March 1967, the US Food and Drug Administration (FDA) licensed Mumpsvax, a vaccine developed by Maurice Hilleman created from the mumps virus infecting his five-year-old daughter, Jeryl Lynn Hilleman. The Mumpsvax vaccine was recommended for routine use in the US in 1977.
The live mumps virus strains were developed in embryonic hens’ eggs and chick embryo cell cultures. This meant that the virus strains were attenuated, and therefore suffered from diminished suitability when used with human cells, though this didn’t stop this strain of the live attenuated mumps virus being further developed into a workable vaccine. The ‘Jeryl Lynn’ strain is still used in vaccines in the US today.
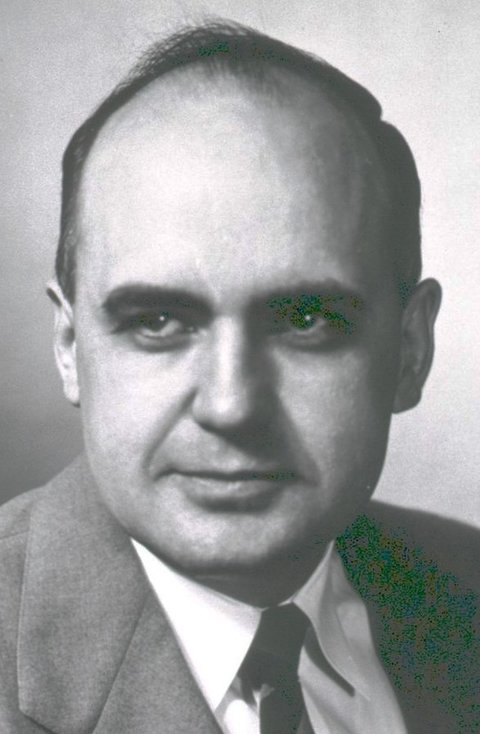
1971
Development of the MMR vaccine
The MMR immunisation vaccine was developed by Hilleman while working at the Merck Institute of Therapeutic Research in Pennsylvania, US, and mixes the live attenuated viruses of measles, mumps and rubella. Hilleman was also the creator of the measles vaccine in 1963, and an improved version in 1968.
While Hilleman also created a rubella vaccine, for the MMR vaccine he used a version developed by Stanley Plotkin at the Wistar Institute. Plotkin used human cells to develop his rubella vaccine, meaning it was better able to protect against the disease than Hilleman’s animal cell-based variety. The MMR vaccine was licenced in 1971, and a second dose was introduced in 1989.
1998
The MMR vaccine autism controversy
In 1998, Andrew Wakefield, at the time a British medical researcher, authored a research paper published in the Lancet medical journal claiming that there was a link between the MMR vaccine and the development of autism, as well as bowel problems.
Wakefield’s study was merely a case report rather than detailed research, and only ever involved 12 children – an incredibly small sample size. The study is now deemed incorrect and fraudulent, but at the time was widely reported on by the media, leading to a sharp drop in vaccination rates in the UK and Ireland and catalysing the anti-vaccination movement. The number of deaths and long-term injuries from mumps and measles rose significantly.
The study has been called one of the most notorious and damaging pieces of literature in the history of modern medicine.

2009
US court refutes claims of autism
The Office of Special Masters of the US Court of Federal Claims, known colloquially as the ‘vaccine court’, was established in 1986 by the National Childhood Vaccine Injury Act, in order to handle vaccine-related injury claims.
In 2009, the court ruled that no evidence had been found to support a link between autism spectrum disorders and vaccines, dismissing suits filed by over 5,300 parents who claimed the MMR vaccine had caused autism in their children.
2010
Wakefield’s autism research dismissed as ‘dishonest’
Several researchers were unable to reproduce Wakefield’s results and in 2004, Sunday Times reporter Brian Deer discovered manipulation of the study’s data, and financial conflicts of interests. Most co-authors withdrew support for the study’s findings, and a thorough investigation by the British General Medical Council (GMC) was carried out into allegations against Wakefield.
On 28 January 2010, the GMC found Wakefield guilty of more than 30 charges, including dishonesty and the abuse of developmentally delayed children. The GMC panel ruled he had ‘failed in his duties as a responsible consultant’, and had acted ‘dishonestly and irresponsibly’. The Lancet journal fully retracted Wakefield’s 1998 study, with the editor-in-chief at the time stating that the publication had been ‘deceived’. Three months later, Wakefield was struck off the UK medical register.
2013
Highest UK MMR vaccination rates
In the UK, universal MMR vaccination became standard in 1988, and in 2013 the UK Health and Social Care Information Centre (HSCIC) reported that during the 2012-2013 period, 92.3% of children had been immunised using the MMR vaccine by their second birthday. This figure was the highest recorded level since its introduction in the UK.
At the time, head of immunisation at Public Health England Mary Ramsay commented that “the findings from HSCIC’s report are a good indication that parents and children are increasingly able to access primary care to receive these vaccinations and to protect their health for the years to come.”

2018
The US mumps resurgence
In 2016, there were several outbreaks of mumps in the US among populations that were already highly vaccinated against the disease, including at Harvard University, where more than 40 people contracted the virus.
The Harvard resurgence brought the issue to the attention of Yonatan Grad, Harvard University assistant professor of immunology and infectious diseases, and Joseph Lewnard, postdoctoral research fellow, who in March this year reported on a resurgence of mumps among vaccinated young adults in the US. The study, carried out by the university’s T.H. Chan School of Public Health, concluded the resurgence was likely due to waning vaccine-derived immunity.
The researchers found that immunity derived from the vaccine lasts an average of 27 years after the final dose is administered, meaning that in addition to the two doses administered to individuals during childhood, a potential third dose at age 18 may be required to maintain immunity into late adulthood.
