Insight
Lyme disease: what's actually going on here?
Chronic Lyme disease is one of the most hotly contested diagnoses in modern medicine – to some doctors it doesn’t even exist, an ailment manufactured by quacks to peddle bogus treatments, and to others it’s one of the most significant invisible illnesses of the modern age. How has so much debate developed, what treatments are on offer, and does anyone really know what’s going on? Chloe Kent reports.
A
‘typical’ case of Lyme disease looks like this: a person in an area populated by the Ixodes scapularis tick gets bitten and picks up a spiral-shaped Borrelia burgdorferi bacterium from the bite. Most people will then develop a target-shaped rash around the bite - known as Erythema migrans - which usually appears within a week, but can take up to a month to materialise. More than 300,000 new cases are reported in the US each year, with a further 65,000 cropping up in Europe.
The bite is often accompanied by flu-like symptoms such as fever, headaches, muscle pain and fatigue. Some patients may not develop or notice a rash, only visiting a doctor when they begin to feel physically unwell, and end up having the infection confirmed by a blood test instead. If the symptoms are ignored the illness can progress to cause more serious neurologic and arthritic problems, known as late disseminated Lyme disease, but even then 30 days of doxycycline should be able to clear things up.
For around 5% – 20% of people with Lyme disease, symptoms such as fatigue and brain fog seem to persist after antibiotic treatment, known as post-treatment Lyme disease syndrome (PTLDS). It’s unknown what causes these symptoms. Some clinicians believe Borrelia burgdorferi triggers an autoimmune response; others hypothesise that PLTDS results from the persistent presence of the bacteria. But studies of PLTDS patients given long-term courses of antibiotics found the drugs performed no better than placebos.
Then, there’s PTLDS’ more controversial cousin – chronic Lyme. Chronic Lyme patients are people who have never had the characteristic bull’s-eye rash or received a reliable positive laboratory test for Lyme disease, but nonetheless maintain Borrelia burgdorferi is responsible for a range of debilitating chronic symptoms they experience.
The supposed symptoms of chronic Lyme encompass a confusing and seemingly endless itinerary of ills. The US Lyme Disease Association lists over 80, including: joint and muscle pain, tenderness in the soles of the feet, sexual dysfunction, menstrual irregularity, incontinence, cystitis, heart palpitations, shortness of breath, brain fog, burning or stabbing sensations, facial paralysis, dizziness, tremors, visual and aural impairments, seizures, depression, insomnia, anxiety, obsessive compulsive disorder, hallucinations, nausea, vomiting, constipation, diarrhoea, fever, fatigue, difficulty swallowing, and swelling around the eyes. The list goes on.
Specialist physicians, who the chronic Lyme community at large have christened Lyme-literate doctors or ‘LLMDs’, support this hypothesis. However, many other figures in the medical establishment maintain that there is no such thing as chronic Lyme. Rather, the label is given to patients with perplexing long-term illnesses by willing clinicians when nothing else seems to fit.
A medical writer, who asked to remain anonymous due to concerns they would face backlash from the online chronic Lyme community, says: “I see chronic Lyme as just a highly evolved form of quackery. It sounds plausible, because it’s based on a real bacterium. We’re storytelling animals and the chronic Lyme story seems compelling. It provides an answer to your problems; it provides hope, feelings of control and a path forward. It also provides an enemy to fight in mainstream medicine, which contradicts the belief in chronic Lyme.”
Lyme disease symptoms
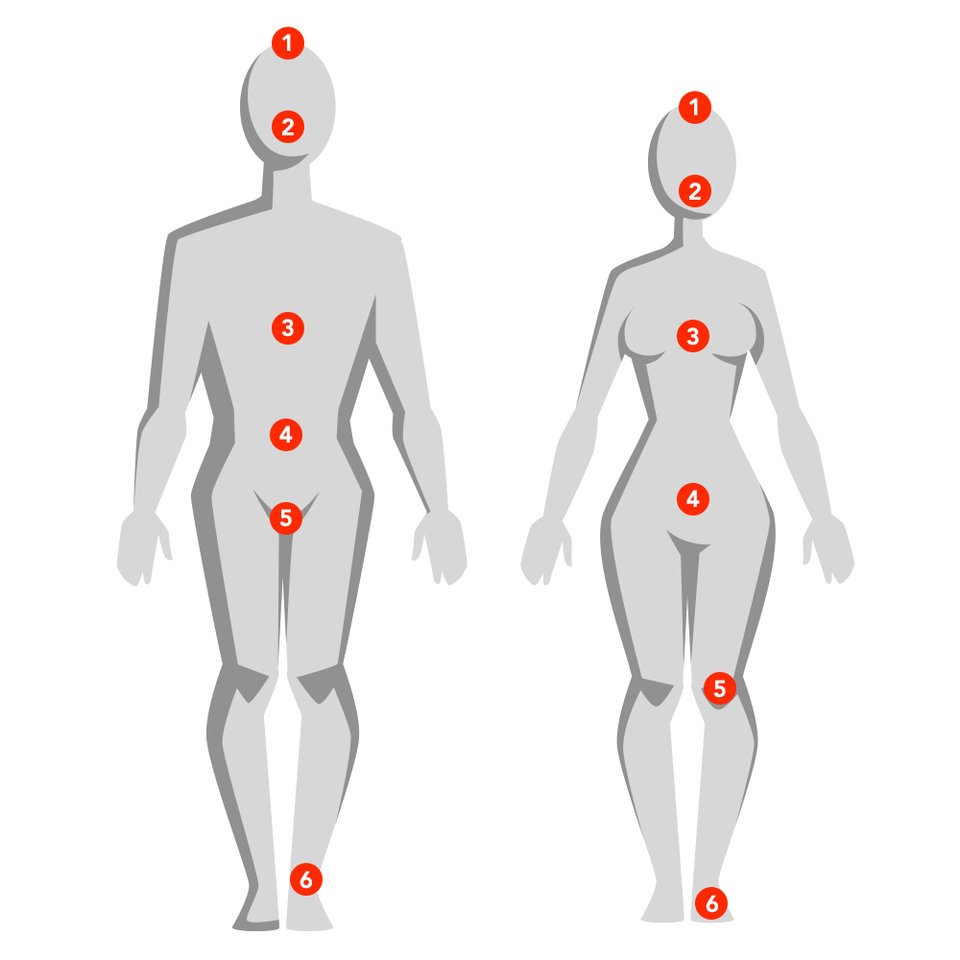
Man
- Obsessive compulsive disorder
- Swelling around the eyes
- Chest pain
- Nausia and vomitting
- Testicular pain
- Tenderness in soles feet
Woman
- Hallucinations
- Facial paralysis
- Shortness of breath
- Menstrual irregularity
- Joint pain
- Burning sensations
Obsessive compulsive disorder
Swelling around the eyes
Chest pain
Nausia and vomitting
Testicular pain
Tenderness in soles of feet
Hallucinations
Facial paralysis
Shortness of breath
Menstrual irregularity
Joint pain
Burning sensations
Icons: Nazar LottieFiles
Hover the icons
Testing, testing, can you find me?
Tests for Lyme disease focus on measuring a patient’s antibodies, rather than the bacteria itself, in a process known as serologic testing. The US Centers for Disease Control (CDC) require two-tiered testing to establish a Lyme disease diagnosis, and both tiers need to come back positive for a diagnosis to be confirmed.
Due to the complexity of the process, there are significant ambiguities in testing best practice across the medical system. Writing in The Atlantic, Meghan O’Rourke describes how her doctor sent her bloods to three labs, two of which gave a positive reading on one part of the test but not the other, and the third of which came back negative on both parts. O’Rourke was informed she probably had Lyme disease, despite not meeting CDC guidelines for a Lyme diagnosis.
Chronic Lyme thus becomes something of a self-fulfilling prophecy. Any ache or ailment could be a symptom and blood test results can be interpreted as indicative of Lyme disease against official guidelines, or even confirm the presence of the disease when it isn’t there.
You really need to wait for six weeks before requesting a blood test.
Bite prevention expert Howard Carter says: “Antibodies to Lyme disease take a few weeks to form – if you have an early test and you’ve got a puncture mark or have removed the tick yourself you can get a false re-assurance, so you really need to wait for six weeks before requesting a blood test.”
Alongside failing to materialise for weeks after a bite, Lyme antibodies can then remain in the bloodstream for years or decades after a Lyme infection has been eradicated, meaning a perfectly healthy person who had Lyme disease as a child might test positive. Other tick-borne diseases, as well as certain viral, bacterial and autoimmune ones, can also activate some of the same antibodies as Lyme disease and lead to false positive test results.
Wayne State University School of Medicine professor of surgery David Gorski, managing editor of the website Science-Based Medicine, says: “Lyme is an infection of a spirochete borne by ticks and it causes a number of symptoms, including the characteristic rash. The point as far as chronic Lyme disease goes is it does not persist after proper treatment with a course of antibiotics.”
Antibiotics and alternative medicine
Of course, LLMDs would beg to differ. Many maintain that one of the best ways to treat chronic Lyme patients is with a long-term course of antibiotics, claiming the typical month-long course of treatment isn’t enough to eradicate the disease in certain individuals.
London’s Lyme Disease Clinic founder and medical director Dr Joshua Berkowitz says: “Long-term treatment with antibiotics is necessary to target and kill all the different pleomorphic forms of the bacteria and parasitic infections associated with chronic Lyme disease. Most of these bacteria have the ability to survive based on different mechanisms and they can easily change their shape and surface.
“They can hide in other body cells and in intracellular spaces, plus they can invade specific tissues like connected tissue where there is no presence of immune cells which can kill them off. With the support of antibiotics we are able to take care of all these escape mechanisms, but it requires long-term treatment to do so.”
Many chronic Lyme patients given a long-term course of antibiotics report feeling better afterwards. But, feeling better on an antibiotic is not a sure fire way to establish that it has actually killed a harmful bacteria, and some argue this approach can actually be dangerous.
Gorksi says: “There are placebo effects. There’s also something known as regression to the mean – most people tend to seek treatment when they’re feeling their worst, but most conditions the symptoms tend to wax and wane. It’s not uncommon at all for symptoms to wane after starting treatment when the treatment isn’t actually responsible for the alleviation of the symptoms.
It’s not uncommon at all for symptoms to wane after starting treatment when the treatment isn’t actually responsible.
“Long-term antibiotics can be downright harmful. It breeds resistant bacteria and antibiotic associated infections happen when your normal bacterial flora gets wiped out. There’s a reason we don’t like to treat people with chronic antibiotics for anything if we can avoid it.”
Neither the CDC, nor the UK National Institute for Health and Care Excellence (NICE), guidelines advocate for long-term antibiotic use to treat Lyme disease. A 2015 review of 33 studies found no evidence suggesting the benefits of extended antibiotic treatment for Lyme disease.
Alongside long-term antibiotics many chronic Lyme patients opt to partake in more wellness-based treatments like supplements, enemas, saunas and steam rooms. While unproven as medicine, if somebody feels popping a turmeric pill and taking a shot of fish oil can improve their symptoms it’s unlikely to cause any real damage. However, more extreme interventions like stem cell transplantation, radiation treatments, and ingesting mercury have sparked more than a few concerns.
One especially popular alternative intervention is ozone therapy. Blood is drawn, injected with ozone gas, and transfused back into the bloodstream, sometimes after being shone under ultraviolet light. Ozone therapy related air embolisms have been implicated in reports of heart attacks, temporary blindness and even some deaths. According to the US Food and Drug Administration (FDA), ozone is a “toxic gas with no known useful medical application.”
A 2015 report in Clinical Infectious Diseases found that the efficacy for these unconventional treatments could not be supported by scientific evidence, and many could potentially be harmful.
Fake diagnosis, not fake disease
One thing everyone can agree upon is that these patients are truly unwell. The fact that they have chronic disabling symptoms is not up for debate, regardless of whether their diagnosis of chronic Lyme disease is accurate, and approaching them with compassion and care is paramount.
Gorski says: “Calling something a fake disease in essence dismisses the symptoms. Calling something a fake diagnosis I think acknowledges that people are experiencing symptoms, that there appears to be something wrong, while at the same time saying that the label that has been put on that constellation of that symptoms is not based in science.”
Calling something a fake disease in essence dismisses the symptoms.
It’s also worth noting that the medical establishment has been wrong many times before, and will be again. Doctors used to believe peptic ulcers couldn’t be caused by bacteria, Ehlers-Danlos syndromes were very rare diseases and smoking was harmless. Perhaps the chronic Lyme sceptics will all be proven irrefutably wrong one day, and this particular tick-borne bacteria is responsible for debilitating chronic illness on a gigantic scale. Or maybe it’s a misdiagnosis of a constellation of conditions with similar symptoms, like chronic fatigue or fibromyalgia. What is vital is that patients are taken seriously when presenting with complex symptoms, and not dismissed by their doctors and sent to hunt for answers elsewhere.