Innovation
No need for animal testing: improving vaccine research with Genoskin
Genoskin has created ex vivo skin models from natural human skin donated by patients undergoing surgery. These models can be used in place of animal models to better predict clinical outcomes and, considering the urgency of the Covid-19 pandemic, Genoskin has made them available to teams working on vaccines for this coronavirus. Allie Nawrat finds out more.
Image: Genoskin
Launched in 2011 in Toulouse, France, Genoskin collects excess human tissue left over from consenting patients undergoing cosmetic surgeries and uses patented techniques to create an ex vivo skin model. The outcome is a 23mm ‘button’ of skin that is kept alive in a culture for around seven days and can be used for research purposes.
Although initially of interest to the cosmetics industry, the pharma and biotech industry has also recognised Genoskin’s potential to support and accelerate drug research and development (R&D), particularly for vaccines and other injectable products.
Genoskin chief commercial officer Eric Merle explains that as these products are immunocompetent, and therefore exhibit immune responses, they can be used as a replacement for the animal skin models that are still the norm for the pre-clinical stages of pharma R&D.
As well as being more ethical, Merle notes that Genoskin’s models are actually clinically superior to animal models. Not only do most animals have a different skin structure from humans, their immunology and immune responses are also divergent, Merle explains. There has been a lot of research in recent years showing that animals have serious limits as models for studying human disease.
Instead, Genoskin’s ex vivo skin allows pharma researchers to get human data – the “holy grail” for drug development – earlier and before studying the drug in real humans. Thereby, Merle argues, Genoskin’s models act as a “de-risking tool”, in addition to being an accelerant. This is crucial given that nine in ten drugs fail in clinical trials, despite being successful in pre-clinical studies in animals.
By better predicting human’s response to drugs and vaccines, Merle argues that Genoskin’s models can also replace some of the initial steps of clinical trials, and consequently those trials may not need to be so big, long or expensive.
Exploring pharma’s interest in Genoskin
Genoskin has worked with big pharma, small biotechs and academic researchers on its skin models. For instance, the company has worked with Sanofi on the responses to the subcutaneous injection of adalimumab, a drug indicated for various autoimmune conditions, in a skin model that reproduces psoriatic lesions.
Genoskin has also worked with the chemicals company Clariant to study mitigating skin ‘inflammaging’ by inhibiting the NLRPE inflammasome and NFkb pathways and with Harvard University on mapping the distributions of metal and metal oxide in ex vivo skin.
The ability to have an immunocompetent tissue that is injectable are two things that set us completely apart.
Industry and academia are not the only stakeholders in the pharma industry to be interested in Genoskin. The company recently met with regulators in both the US and Europe, which are interested in moving away from animal testing and the possibilities of the alternatives.
Interest from the pharma industry in Genoskin peaked with the launch of the world’s first injectable platform; this model can receive injections because it contains the hypodermis or fatty layer between the dermis and epidermis. “The ability to have an immunocompetent tissue that is injectable are two things that set us completely apart and have transformed our company in the past two years,” notes Merle.
Due the urgency of resolving the Covid-19 pandemic, which has killed more than one million people globally to date, Genoskin moved to make its ex vivo skin models available to teams researching Covid-19 vaccines with the aim of accelerating and improving progress.

Image: Genoskin
Genoskin’s contribution to Covid-19 research
On the back of a virtual meeting organised by the Biotech International Organisation on Covid-19, early into the first wave of the pandemic, Genoskin launched a preferred access programme for its entire portfolio.
Despite being a small company and the complicated, time-constrained logistics of producing its ex vivo skin models, Genoskin has managed to turn every meeting it has had with researchers into something productive. Unfortunately, Merle was unable to share precisely who the team was working with on its Covid-19 projects.
Central to why Genoskin’s model is a positive to researchers, according to Merle, is that Covid-19 “research is moving very quickly [so] timeliness becomes critical”, and therefore getting human data as early as possible is of real benefit here.
The first steps of vaccination take place in the skin – the triggering of the immune cells.
With regard to vaccines, Merle explains, Genoskin’s models are particularly helpful because “the first steps of vaccination take place in the skin – the triggering of the immune cells”, as well as signs of toxicity, including skin cell death and injection site reactions. These can be detected and characterised in the company’s models with the help of algorithm-based advanced imaging technology, thereby indicating initial safety and efficacy results for the vaccine.
Genoskin chief scientific officer Nicolas Gaudenzio explains the science behind the skin’s key role in these early steps of vaccination.
“The skin is a tissue rich in antigen presenting cells (APCs). These APCs will not only allow the recruitment of circulating [immune] cells at the vaccine site (e.g. monocytes, neutrophils, T lymphocytes), but also they will migrate into the secondary lymphoid organs to initiate an adaptive cellular and humoral immune response that will be at the origin of vaccine protection,” Gaudenzio notes. Therefore, a safe and effective vaccine must be able to properly target and activate the APCs in the skin to induce “an effective and sustainable adaptive response over time”.
On the back of this Covid-19 vaccine programme, Genoskin plans to launch a full vaccine platform that will “allow customers to screen [their vaccines] against what is already known vaccines”. Therefore, this allows for better predictions of comparisons between novel vaccines and products already on the market.
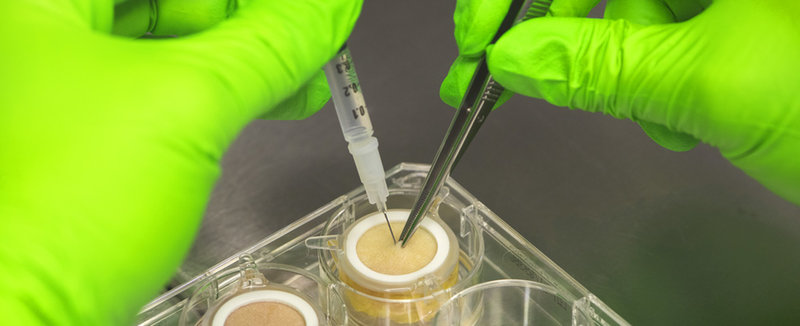
Image: Genoskin
Not the same as an actual human: overcoming Genoskin’s limitations
Merle is very clear that, obviously, these small skin models cannot replace clinical studies in human beings. Although researchers can get a picture of the first steps and an indication of toxicity and efficacy of the vaccine over the seven-day period these models can be reliably kept alive for, Genoskin’s product is a not a full organism and it cannot model what happens with the immune response outside of the skin.
One of the main limits of the model is that it is disconnected from the rest of the body.
However, Genoskin is working on starting to overcome shortcomings of its system. Merle notes that the company has recently filed a patent to resolve one of the main limits of the model, which is that it is disconnected from the rest of the body, so there’s no blood flow going through it. The company is going to recreate this flow and is going to test this model with a pharma partner.
Genoskin is very motivated to continue expanding and improving its capabilities because of the generosity of patients who donated their skin tissue to the company and its research partners. “We owe it to their generosity to actually generate as much characterisation on this tissue as possible,” concludes Merle.